Topics to be Learn
- Introduction
- Immunity
- Structure of antibody
- Common human diseases
- Adolescence
- Addiction
- Drugs abuse
Health:
- Defined by WHO as the state of complete physical, mental, and social wellbeing and not just absence of disease.
- Involves metabolic and functional efficiency of living organisms.
Hygiene: Science of rules of health.
- Essential for good health: Hygienic balanced diet, clean drinking water, personal and community hygiene, regular physical exercise, knowledge about diseases and their effects, proper waste disposal, and vector control.
Human Body Health System:
- Exposed to various foreign bodies including pathogens like bacteria, viruses, etc.
- Immune system protects against these pathogens.
- Resistance and prevention of damage or disease through defence mechanisms.
- Despite exposure, most remain healthy due to effective immune response.
Immune System:
- Protects from various pathogens or infectious agents.
- Edward Jenner: Pioneer of immunity concept, developed Cowpox vaccine.
- Resistance: Prevents damage or disease via defence mechanisms.
- Immunity: host's resistance to infections caused by pathogens.
- Immunology: Study of immune system and its responses.
- Antigen: Foreign substance stimulating immune response.
- Antibody: Protective chemicals produced in response to antigens.
Types of Immunity:
- Innate Immunity: Natural, non-specific.
- Acquired Immunity: Developed through exposure to pathogens or vaccination.
Innate Immunity:
- Natural, inborn immunity against microorganisms.
- Non-specific, not dependent on previous exposure.
- Mechanisms: Anatomical, physiological, phagocytic, and inflammatory barriers.
Barriers of Innate Immunity:
1) Epithelial Surface:
- Skin and mucous coverings protect against pathogens.
- Sebaceous glands produce bactericidal and fungicidal secretions.
- Respiratory tract's mucosa prevents microorganism entry.
- Hair in nasal passage arrests inhaled particles.
- Mucus lining epithelium catches particles, swept back to pharynx.
- Saliva inhibits microorganisms, gastric secretions destroy in stomach.
- Urine flushing eliminates bacteria, semen has antibacterial substances.
2) Antimicrobial Substances:
- Complement system with 30 serum proteins eliminates pathogens.
- Interferons released by virus-infected cells, stimulate immune response.
- White blood cells (WBCs) stimulate other cells.
3) Cellular Factors:
- Phagocytic cells ingest and destroy pathogens.
- Microphages and macrophages remove foreign particles.
- Natural killer (NK) cells defend against viral infections and tumors.
4) Fever:
- Raises body temperature, accelerates physiological processes.
- Stimulates interferon production.
5) Acute Phase Proteins (APPs):
- Increased during infection or injury.
- Enhance host resistance, prevent tissue injury, promote repair.
Acquired Immunity or adaptive immunity acquired during lifetime due to infections.
- Specific or adaptive immunity fights specific antigens, takes time to activate, seen only in vertebrates.
- Involves formation of antibodies from destruction of foreign antigens.
- Unique Features: Specificity, diversity, discrimination between self and non-self, and memory.
Types of Acquired Immunity:
1) Active Immunity:
- Produced in response to pathogens or antigenic stimuli.
- Long-lasting.
- Body produces its own antibodies.
- Natural: Obtained from infections.
- Artificial: Obtained from vaccinations, containing dead or attenuated pathogens.
2) Passive Immunity:
- Produced due to transferred antibodies.
- Short-lived.
- Antibodies given from outside.
- Natural: Antibodies from mother to baby via placenta or colostrum.
- Artificial: Vaccines containing pre-made antibodies, often derived from other animals.
Cells of the Immune System:
(a) Lymphocytes:
- Main cells of the immune system.
- Arise from haemocytoblasts in the liver (foetus) and bone marrow (adult).
1) Bursa/B-Lymphocytes:
- Differentiate in gut-associated bursal lymphoid tissues (e.g., Tonsils, Peyer’s patches).
- Form humoral or antibody-mediated immune system (AMIS).
2) Thymus/T-Lymphocytes:
- Differentiate in the thymus.
- Form cell-mediated immune system (CMIS).
Mechanism of Response of T-Lymphocytes to Antigens: Upon antigen contact, T-lymphocyte forms clones performing different functions.
- Four Types of T-Lymphocytes:
- Helper T-cells: Produce lymphokines.
- Killer T-cells (Cytotoxic T-cells): Directly attack and destroy invading microbes.
- Suppressor T-cells: Suppress entire immune system against own body cells.
- Memory T-cells: Remember antigens.
Mechanism of Action of B-Lymphocytes to Antigens:
- Sensitization: Directly sensitized by antigens and helper T-cells.
- Activation:
- Activated B-lymphocyte rapidly multiplies.
- Produces clone of plasma cells and memory B-cells.
- Production of Antibodies:
- Plasma cells produce specialized glycoproteins called antibodies.
- Antibodies circulate in body fluids (blood and lymph).
- Functions of Antibodies:
- Agglutination: Clumping of particles, aiding in phagocytosis by phagocytes.
- Opsonization: Coating of bacteria, facilitating their engulfment by macrophages.
- Neutralization: Inactivation of toxins released by bacteria (e.g., tetanus toxin).
- Specificity: Each antibody is specific for a particular antigen.
(b) Antigen Presenting Cells:
- Engulf invading pathogens and process antigens.
- Deliver a stimulatory signal necessary for activation of helper T-cells.
Vaccination: Administration of inactivated pathogen or antigenic protection of a particular pathogen to provide immunity.
Vaccine: Inactivated pathogen or antigens of a specific disease.
Preparation and Administration:
- Components: Inactivated pathogen, protein or sugar from pathogen, dead form of pathogen, toxoid from pathogens, or attenuated pathogen.
- Process: Administered to protect against a particular pathogen.
- Purpose: Teaches the immune system to recognize and eliminate pathogenic organisms.
- Response: Body produces antibodies in response to vaccine.
- Primary Prevention: Reduces chances of illness by preparing the body before exposure to the pathogen.
Benefits of Vaccination:
- Disease Control: Controls spread of diseases like measles, polio, tetanus, and whooping cough.
- Epidemic Control: Prevents epidemic outbreaks if all people are vaccinated.
- Eradication: Some diseases like smallpox and polio have been completely eradicated through vaccination.
Structure of Antibody:
- Definition: Glycoproteins highly specific to specific antigens.
Production:
- Produced by plasma cells, formed by B-lymphocytes.
- Approximately 2000 antibody molecules formed per second by plasma cells.
Physical Structure:
- Shape: 'Y'-shaped molecule.
- Composition: Four polypeptide chains - two heavy (H) chains and two light (L) chains.
- Disulfide Bonds: Hold polypeptide chains together, forming 'Y' structure.
- Hinge: Region holding arms and stem of antibody.
Regions:
- Variable Region: Contains paratope, the antigen-binding site.
- Constant Region: Region with constant structure.
Functionality:
- Antigen Binding: Variable regions bind to specific antigens, forming antigen-antibody complex.
- Bivalency: Antibodies are bivalent, carrying two antigen-binding sites.
Formation of Antigen-Antibody Complex:
- Specificity:
- Between antigen and antibody.
- Each antibody specific for a particular antigen.
- Antigenic Determinants: Combining sites on antigens, called antigenic determinants or epitopes.
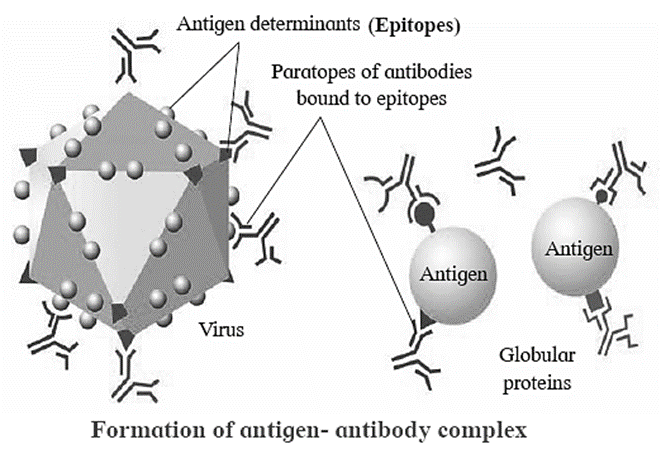
- Paratopes: Corresponding antigen binding sites on antibodies.
- Variable Regions:
- Antigen binding sites located on variable regions of antibodies.
- Small variations in variable regions make each antibody highly specific for a particular antigen.
- Recognition:
- Antibody recognizes specific antigen due to variable region.
- Binds to specific antigen in a lock-and-key manner.
- Complex Formation: Antibody binds to specific antigen, forming antigen-antibody complex.
Antigen on Blood Cells:
- Overview: Responsible for different blood groups.
- Variety:
- About 30 known antigens on human red blood cells.
- Determine blood group types such as ABO, Rh, Duffy, Kidd, Lewis, MNS, Bombay.
- Genetic Determination: Different blood groups determined genetically by the presence of specific antigens.
- Landsteiner's Discovery:
- Landsteiner identified two antigens on human red blood cells: Antigen A and Antigen B.
- Antigen D determines Rh status: Rh positive if present, Rh negative if lacking.
- Implications: Determine blood group types and compatibility for transfusions.
- Agglutination Reactions: Antigens on RBCs and antibodies in serum can cause agglutination reactions if incompatible.
- Transfusion Protocol:
- Blood groups checked thoroughly before transfusion to ensure compatibility.
Blood Group Systems: Include ABO, Rh, Duffy, Kidd, Lewis, MNS, Bombay blood group, etc.
ABO Blood Group System:
Overview:Determines blood groups by antigens on red blood cells (RBCs).
Blood Groups: Four types: A, B, AB, O.
Blood Group Characteristics:
- A: Antigen A on RBCs, antibodies 'b' in plasma.
- B: Antigen B on RBCs, antibodies 'a' in plasma.
- AB: Antigens A and B on RBCs, no antibodies in plasma.
- O: No antigens A or B on RBCs, antibodies 'a' and 'b' in plasma.
Blood Transfusion:
- Compatibility crucial during transfusion.
- O: Universal donor.
- AB: Universal recipient.
ABO Blood Groups in Man Chart:
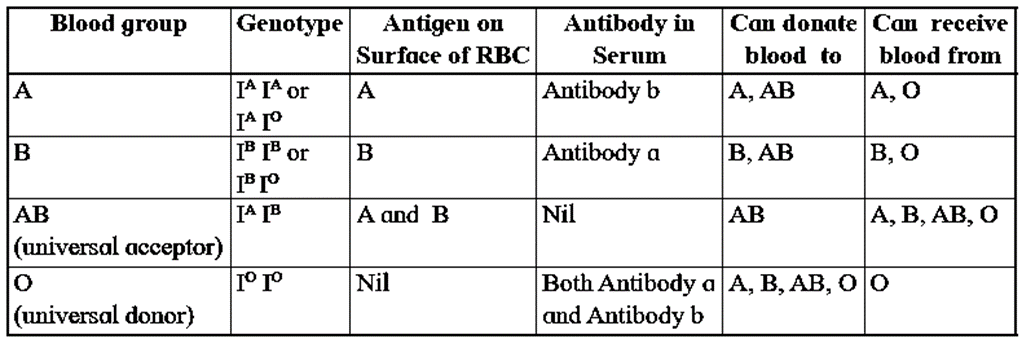
- Key Discoveries:
- Karl Landsteiner: Discovered A, B, and O blood groups in 1900.
- Decastello and Sturli: Discovered blood group AB in 1902.
Rh Factor:
- Definition: Term adapted from Rhesus monkey.
- Rhesus Monkey: Antigen D present on their RBCs.
- Discovery: Landsteiner and Wiener discovered the antigen, termed it Rh factor.
- Rh Positive and Rh Negative:
- Rh positive: Individuals with Rh factor or D antigen.
- Rh negative: Individuals lacking D antigen or Rh factor.
- Immunogenic Response: Rh (D) antigen induces strong immunogenic response in Rh negative individuals.
- Haemolytic Diseases of the Newborn (HDN): Occurs when Rh-negative mother conceives Rh-positive foetus.
Common Human Diseases:
Definition of Disease:
- Condition of disturbed or deranged functioning of one or more organs or organ systems caused by infections, defective diet, or heredity.
Classification:
- Congenital Diseases:
- Present from birth.
- Caused by genetic abnormality or metabolic disorder.
- Some incurable but modern research offers treatments like gene therapy, enzyme replacement therapy.
- Acquired Diseases: Develop after birth.
- Communicable or Infectious Diseases: Spread from person to person.
- Non-communicable or Non-infectious Diseases: Not spread from person to person.
Communicable or Infectious Diseases:
- Congenital Diseases:
- Definition: Transmitted from infected person to healthy person.
- Transmission: Spread through pathogens.
- Inheritance: Not inherited from parental generation to offspring.
- Vectors: Major role played by vectors in disease transmission.
- Treatment: Conventional methods like antibiotics and drugs.
- Development: Acute diseases develop suddenly due to infections.
- Examples: Pneumonia, Tuberculosis, AIDS, Typhoid, Cholera, Malaria.
Non-communicable or Non-infectious Diseases:
- Definition: Not passed from one person to another.
- Transmission: Do not spread through pathogens.
- Inheritance: Some, like cancer, can be inherited from parental generation to offspring.
- Causes: Allergy, illness, malnutrition, abnormalities in cell proliferation, changes in lifestyle, environment.
- Treatment: Conservative treatment or surgery over a long period.
- Development: Chronic diseases develop and persist for a long time.
- Examples: Cancer, Rickets, Allergies, Kwashiorkor, Diabetes, Heart disease.
1) Malaria (Type-Protozoan):
Mode of Transmission: Transmitted through female Anopheles mosquito, acting as a vector.
Causative Organisms:
- Disease caused by protist - Plasmodium.
- Four species: P. vivax, P. falciparum, P. ovale, P. malariae.
Symptoms:
- Fever, shivering, joint pain, vomiting, anaemia, haemoglobinuria, retinal damage, convulsions.
- Cyclical occurrence of sudden coldness followed by rigor, fever, and sweating.
- Enlarged spleen, severe headache, cerebral ischemia, enlarged liver, hypoglycaemia, haemoglobinuria with renal failure in severe infections.
Diagnosis and Treatment:
- Blood smear testing, nucleic acid amplification technique.
- ACT therapy: Various combinations of artesunate, sulfadoxine, pyrimethamine, quinine.
Preventive Measures:
- Prevent mosquito bites: mosquito nets, insect repellents.
- Mosquito control measures: insecticide spraying, stagnant water drainage, Gambusia fish release.
- Vaccine development ongoing.
2) Amoebiasis or Amoebic Dysentery (Type-Protozoan):
- Mode of Transmission: Faecal-oral route, contact with dirty hands/objects, anal-oral contact, contaminated food/water.
- Causative Organisms:
- Spread through ingestion of cyst form of Entamoeba histolytica.
- Cyst is found in faeces; non-encysted amoebae are trophozoites.
- Trophozoites rarely source new infections; infection may remain asymptomatic.
- Symptoms:
- Diarrhoea, flatulence, stool with mucus, abdominal cramps.
- Sticky stool with mucus and blood.
- Hepatomegaly if amoebae form cysts in liver; liver abscess may occur with fever and right abdominal pain.
- Diagnosis and Treatment:
- Microscopic stool examination.
- Metronidazole and Tinidazole.
- Preventive Measures:
- Home Level:
- Washing hands with soap after toilet use/diaper change.
- Proper bathroom/toilet cleaning.
- Avoiding raw vegetables in endemic areas.
- Boiling/drinking purified water.
- Endemic Level:
- Avoiding street foods in public places.
- Good sanitary practices, sewage disposal/treatment.
- Sedimentation/filtration of water supplies.
- Avoiding shared towels or face washers.
3) Ascariasis (Type-Helminth):
- Mode of Transmission:
- Contaminated food/drinks with Ascaris eggs.
- Eggs hatch in host intestine; larvae enter organs through circulation.
- Adults settle in host's digestive system.
- Causative Organisms:
- Ascaris lumbricoides.
- Endoparasite, roundworm, or nematode.
- Symptoms:
- Appearance of eggs in stools after 60-70 days.
- Larval ascariasis symptoms in 4-16 days.
- Gastrointestinal discomfort, colic, vomiting, fever, live worms in faeces.
- Pulmonary symptoms, pneumonitis, neurological disorders.
- Loss of appetite, weight loss, intestinal obstruction risk.
- Larvae migration may cause eosinophilia.
- Diagnosis and Treatment:
- Anti-helminthic drugs like Piperazine, Mebendazole, Levamisole, Pyrantel.
- Microscopic stool examination.
- Preventive Measures:
- Use proper toilet facilities.
- Safe excreta disposal.
- Protect food from dirt/soil; wash vegetables/fruits before eating.
- Hand hygiene and safe food practices.
- Use pharmaceutical drugs like Mebendazole, Albendazole.
4) Filariasis or Elephantiasis (Type-Helminth Nematode endo-parasite):
- Mode of Transmission:
- Parasite Wuchereria bancrofti transmitted by female Culex mosquito.
- Larvae leave mosquito, penetrate human skin, undergo moulting, and settle in lymphatic system.
- Results in lymphatic filariasis; lymph vessels/nodes enlarge, causing elephantiasis.
- Causative Organisms:
- Lymphatic Filariasis: Wuchereria bancrofti, Brugia malayi, Brugia timori.
- Subcutaneous Filariasis: Loa loa, Mansonella spp.
- Serous cavity Filariasis: Mansonella spp.
- Symptoms:
- Oedema, skin/tissue thickening due to impaired lymphatic drainage.
- Extremities (legs, arms, breasts, scrotum) affected, lymph vessels/nodes swollen.
- Elephantiasis: limbs swell like elephant legs.
- Lymphoedema: tissue swelling due to lymph fluid accumulation.
- Hydrocele: testis enlargement from lymphatic fluid accumulation.
- Diagnosis and Treatment:
- Diethyl-carbamazine citrate twice daily for three weeks, then for five days every six months.
- Effective against filarial worms.
- Preventive Measures:
- Mosquito eradication to control filariasis.
- Use mosquito nets and repellents in mosquito-prone areas.
5) Typhoid (Type-Bacterial):
- Mode of Transmission:
- Gram-negative bacterium Salmonella typhi.
- Food and waterborne; transmitted by poor hygiene, sanitation, houseflies, and cockroaches.
- Causative Organisms:
- Salmonella typhi.
- "O" antigen (lipopolysaccharide) and flagella contribute to pathogenicity.
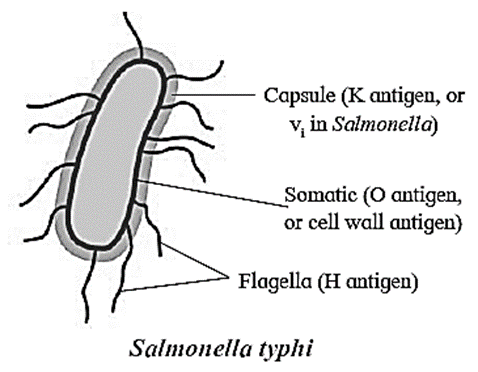
- Symptoms:
- Prolonged high fever, nausea, fatigue, headache.
- Abdominal pain, constipation/diarrhoea, rose-coloured rash.
- White tongue coat, cough, anorexia, breathlessness, irregular heartbeats.
- Diagnosis and Treatment:
- Widal test for diagnosis.
- Surgical gall bladder removal in severe cases.
- Antibiotics like Chloramphenicol.
- Preventive Measures:
- Cleanliness, safe food, avoiding roadside food.
- Vaccines: Oral (Ty21a) and Injectable (Typhim Vi, Typherix).
6) Pneumonia (Type: Bacterial, Viral, Physical, Burns):
- Mode of Transmission: Direct contact, droplets infection, shared items.
- Causative Organisms:
- Virus: Influenza, adenovirus, parainfluenza, RSV.
- Bacteria: Streptococcus pneumoniae.
- Fungal: Pneumocystis jirovecii, Pneumocystis carinii.
- Symptoms:
- Cough, yellow/greenish sputum.
- High fever, shortness of breath.
- Chest pain with deep breath or cough, loss of appetite, fatigue.
- Inflammation of respiratory passage and lungs.
- Diagnosis and Treatment:
- Tailored treatment based on the pathogen.
- Antibiotics like Benzyl penicillin, Ampicillin, Chloramphenicol for bacterial pneumonia.
- Preventive Measures:
- Vaccination for both children and adults.
- Vaccines against Haemophilus influenzae and Streptococcus pneumoniae in the first year of life.
- (7) Common cold (Type-Viral) :
- Mode of transmission :
- Transmitted through droplet infections:
- Nasopharyngitis
- Acute viral rhinopharyngits
- Acute coryza or a cold
Causative organisms :Rhinoviruses and Corona-viruses
Symptoms :
- Cough. sore throat, runny nose and fever.
- Sneezing with nasal congestion, Conjunctivitis (red eyes)
- Muscle rashes, fatigue, headache
- Shivering and loss of appetite
Diagnosis and Treatment :
- No medicines.
- Painkiilers and paracetamol may help
- Homemade remedies more common.
Preventive measures :
- To keep away from persons having common cold
- Hand-wash using soap and water.
- Handkerchief to cover the nose and mouth during coughing and sneezing.
- Alcohol based hand sanitizer can also be used.
8) Ringworm Dermatophytosis (Type: Fungal):
- Mode of Transmission: Sharing clothes, comb of infected person, close contact.
- Causative Organisms: Fungal Species: Trichophyton, Microsporum.
- Symptoms:
- Enlarged, red rings on skin.
- Intense itching, dry scaly lesions on various body parts.
- Thick, discoloured, disfigured nails.
- Fungal infection usually begins between the toes.
- Diagnosis and Treatment:
- Physical examination.
- Drugs like Nystatin, fluconazole, itraconazole, etc.
- Preventive Measures:
- Avoid close contact and sharing clothes/equipment.
- Wash clothes in hot water with fungicidal soap.
9) Dengue (Type: Viral):
- Mode of Transmission:
- Vector: Female Aedes mosquito.
- Dengue virus is transmitted when mosquitoes feed on infected individuals.
- Causative Organisms: Four closely related dengue viruses.
- Symptoms: High fever, Vomiting, Severe headache, Decrease in platelet count.
- Diagnosis and Treatment: Blood test, Physical examination.
- Preventive Measures: Mosquito control, Eliminate stagnant water in containers.
10) Cancer:
- Abnormal, uncontrolled cell division leads to the formation of tumors.
- When tumors are malignant, they are described as cancer and can invade other tissues.
Key Terms:
- Neoplasm: Masses of tissue formed due to uncontrolled cell division.
- Oncologists: Specialists in the study, diagnosis, treatment, and prevention of cancer.
Types of Tumors:
- Benign Tumor:
- Localized and does not spread.
- Enclosed in connective tissue sheath.
- Compresses surrounding normal tissue.
- Can be surgically removed.
- Usually not fatal except for brain tumors.
- No metastasis.
- Well-differentiated.
- Slow and progressive growth.
- Malignant Tumor:
- Starts locally but spreads rapidly.
- Not enclosed in connective tissue sheath.
- Invades and destroys surrounding tissue.
- Requires further treatment after removal.
- Often fatal.
- Shows metastasis.
- Poorly differentiated.
- Rapid and erratic growth.
Symptoms of Cancer:
- Presence of lump or tumor.
- White patches in the mouth.
- Changes in warts or moles on the skin.
- Swollen or enlarged lymph nodes.
- Vertigo, headaches, or seizures if cancer affects the brain.
- Coughing and shortness of breath if lungs are affected.
Types of Cancer:
1) Carcinoma:
- Cancer of epithelial tissue covering or lining body organs.
- Examples: breast cancer, lung cancer, stomach cancer, skin cancer.
2) Sarcoma:
- Cancer of connective tissue.
- Examples: osteosarcoma (bone cancer), myosarcoma (muscle cancer).
3) Lymphoma:
- Cancer of lymphatic tissue.
- Affects lymph nodes, spleen, and immune system tissues.
4) Leukemia:
- Blood cancer.
- Excessive formation of leukocytes in the bone marrow.
- Types: monocytic leukemia, lymphoblastic leukemia.
5) Adenocarcinoma:
- Cancer of glandular tissues.
- Examples: thyroid cancer, pituitary cancer.
Causes of Cancer:
- Chemicals: Nicotine, caffeine, polycyclic hydrocarbons, sex hormones.
- Radiation: X-rays, gamma rays, ultraviolet rays.
- Viruses: Epstein-Barr virus (EBV), human papillomavirus (HPV).
- Oncogenes: Cellular oncogenes or proto-oncogenes.
- Addiction: Cigarette smoke, tobacco, alcohol, drugs like marijuana.
Cancer Treatment:
- Chemotherapy: Anticancer drugs inhibiting DNA synthesis.
- Radiotherapy: Radiations from radioactive materials.
- Surgery: Removal of cancerous tissue.
- Immunotherapy: Biological response modifiers.
- Supportive Therapy: Enhancing quality of life and treating symptoms.
11) AIDS:
- AIDS: Acquired immunodeficiency syndrome, caused by HIV (Human immunodeficiency virus).
- Structure of HIV:
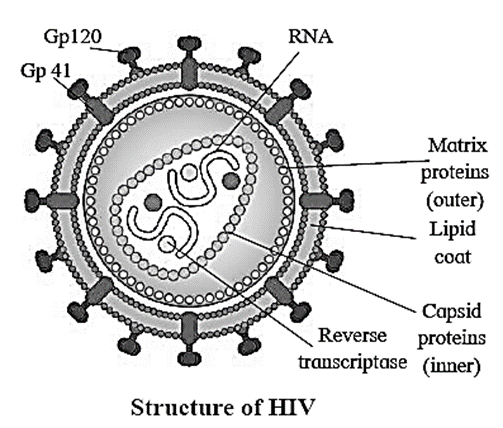
- Spherical, 100 to 140 nm diameter.
- Contains two ss RNA molecules and reverse transcriptase enzymes.
- Outer layer: matrix protein (p17) with lipid and glycoproteins GP120 and GP41.
- Inner layer: capsid protein (p24).
- Transmission of Virus:
- Unsafe sexual contact (oral, vaginal, anal).
- Blood transfusions, sharing needles.
- Transplacental and breastfeeding.
- Accidental needle injury, organ transplantation.
- Transmission through urine, tears, saliva, breast milk, vaginal secretions.
Effects of HIV/AIDS:
- Weakens the immune system.
- Increases vulnerability to opportunistic infections, neurological disorders, and malignancies.
Concentration of HIV: Blood, semen, and cerebrospinal fluid (CSF) have the highest concentration, with lesser extent in tears, milk, urine, saliva, cervical, and vaginal secretions.
Clinical Manifestation of AIDS:
- Stage I: Initial infection with the virus, antibody formation (2-8 weeks after infection).
- Stage II: Asymptomatic carrier stage, incubation period (6 months to 10 years).
- Stage III (ARC - AIDS Related Complex):
- Recurrent fever for over a month.
- Fatigue.
- Unexplained diarrhea.
- Night sweats.
- Shortness of breath.
- Loss of over 10% body weight.
- Stage IV (Full-blown AIDS):
- End stage of HIV infection.
- Life-threatening opportunistic infections (pneumonia, tuberculosis, Kaposi sarcoma).
- Laboratory Diagnosis:
- ELISA (Enzyme-Linked Immunosorbent Assay) detects HIV antibodies.
- Western Blot confirms results and eliminates false positives.
- Treatment:
- No cure for AIDS.
- Antiretroviral drugs reduce viral load and prolong life (e.g., TDF, EFV, Lamivudine).
Preventive Measures:
- Educating high-risk groups about HIV transmission.
- Use disposable needles and syringes.
- Avoid risky sexual habits.
- Avoid sharing items contaminated with blood.
- Screen blood donors, organ donors, and patients undergoing dialysis.
- Regularly screen pregnant women and those considering pregnancy.
Adolescence
- Definition: Transitional stage of physical and mental development during puberty, spanning from 13 to 19 years.
Stages of Adolescence:
Early Period (10 to 14 years):
- Appearance of secondary sexual characteristics.
- Rapid physical growth.
- Concrete thinking.
- Self-exploration and developing body image.
- Formation of intense friendships.
Middle Period (15 to 17 years):
- Completion of secondary sexual characteristics.
- Slowed physical growth.
- Abstract thinking emerges.
- Development of long-range thinking and leadership skills.
- Peer group influence and attraction testing.
Late Period (18 to 19 years):
- Total physical maturity.
- Full abstract thinking.
- Individual relationships over peer groups.
- Stable relationships and transition to adulthood.
Physical Changes of Adolescence:
- Growth Spurt: Rapid increase in height and weight.
- Sexual Development: Onset of puberty and reproductive maturity.
- Emotional and Social Changes: Transition from dependence to independence, exploring identity and relationships.
Mental Health and Adolescence
- Common Problems:
- Confusion, irritation, moodiness, frustration.
- Decreased concentration and hyperactivity.
- Anger, leading to lifestyle issues like obesity and addiction.
- Psychoses with delusions and hallucinations.
- Amnesia, bulimia, anxiety, anorexia nervosa, depression, illusions, and hallucinations.
- Cognitive, emotional, behavioral, physical, and attitudinal changes.
- Parental communication and environment influence adult personality.
- Improper peer pressure may lead to addictions.
Treatment:
- Counseling is preferred over medication, respecting children's rights.
- Mental Health Gap Action Programme (mhGAP) provides WHO guidelines.
- Parental relations are crucial in treatment.
Addiction
- Definition: Compulsive substance use despite harmful consequences.
- Addictive Substances: Alcohol, opioids, cocaine, nicotine, and behaviors like gambling.
- Neurobiological Features:
- Brain pathways of reward and reinforcement are involved.
- Dopamine release during motivation.
- Neurological changes are reversible after discontinuation.
- Causes of Substance Abuse in Adolescence:
- Parental neglect and lack of supervision.
- Poor communication between parents and children.
- Family conflicts and lack of rules.
- Favorable parental attitudes towards substance use.
- Risk-taking behavior.
- Measures to Control Drug Abuse:
- Prevention through education and counseling.
- Avoiding overpressure and setting realistic expectations.
- Channelizing energy into constructive activities like sports and studies.
Drug Abuse:
Effects:
- Drug and alcohol use among youth leads to harmful effects and dangerous behavior patterns.
- These habits are hazardous for individuals and society.
Commonly Abused Drugs:
1. Opioids (Smack, Heroin):
- Bind to opioid receptors in the central nervous system and gastrointestinal tract.
- Heroin, also known as smack, is chemically diacetyl morphine, extracted from the poppy plant.
- Depressant that slows down body activity.
2. Cannabinoids (Marijuana, Hashish, Charas, Ganja):
- Interact with receptors in the brain.
- Inhalation and ingestion affect the cardiovascular system.
- Obtained from Cannabis sativa plant.
3. Cocaine (Crack, Coke):
- Alkaloid obtained from the coca plant.
- Increases dopamine neurotransmitter levels.
- Excessive dosage causes extreme happiness, irritability, and paranoia.
4. Hallucinogens (Mind-Expanding Drugs):
- Alkaloids causing daydreaming.
- Lycergic acid and cannabis are hallucinogenic substances.
- Plants like Atropa belladonna and Datura spp. also have hallucinogenic properties.
- Hallucinations are unreal perceptions due to nervous system disorders.
Addiction and Dependence:
- Inherent addictive nature of alcohol and drugs leads to psychological attachment.
- Repeated use increases receptor tolerance.
- Addicted individuals engage in self-destructive behavior.
- Withdrawal symptoms include anxiety, trembling, nausea, and sweating when substances are discontinued.
Effects of Drug/Alcohol Abuse:
- Reckless behavior: Drug and alcohol abuse can lead to reckless behavior, vandalism, and violence.
- Overdose: Excessive doses of drugs/alcohol can result in coma or death due to respiratory failure, heart failure, or cerebral hemorrhage.
- Weird combinations: Mixing drugs and alcohol can increase the risk of overdose and death.
Warning Signs of Drug and Alcohol Abuse Among Youth:
- Drop in academic performance: Decline in school/college performance.
- Unexplained absences: Frequent absences from school/college without explanation.
- Lack of personal hygiene: Neglect of personal hygiene, withdrawal from social activities, isolation, depression, and fatigue.
- Aggressive behavior: Increased aggression, rebellion, and deterioration of relationships with family and friends.
- Loss of interest: Loss of interest in hobbies and activities previously enjoyed.
- Sleep and eating disturbances: Changes in sleeping and eating habits, fluctuations in weight and appetite.
- Involvement in crime: Engaging in criminal activities to obtain money for drugs/alcohol.
Other Hazards:
- Infections: Intravenous drug users are at risk of acquiring serious infections such as HIV and hepatitis B.
Long-Term Effects:
- Health issues: Loss of balance, liver cirrhosis, pancreatitis, and other chronic health conditions.
- Heavy drinking in adulthood: Substance abuse during adolescence may lead to continued heavy drinking in adulthood.
- Damage to nervous system and liver: Chronic drug/alcohol use can damage the nervous system and liver, leading to conditions such as cirrhosis. Substance use during pregnancy can also negatively affect the fetus.
Performance Enhancers:
Performance enhancers refer to certain drugs used by athletes to improve their athletic performance during competitions. These substances are often misused and may have harmful effects on the body.
Types of Performance Enhancers:
- Narcotic analgesics: Pain-relieving drugs that can mask pain and discomfort, allowing athletes to push themselves harder during training and competitions.
- Anabolic steroids: Synthetic substances that mimic the effects of testosterone, promoting muscle growth, strength, and endurance.
- Diuretics: Drugs that increase urine production, leading to water loss and temporary weight reduction, which may be advantageous in sports with weight categories.
- Hormones: Certain hormones, such as growth hormone and erythropoietin (EPO), may be used to enhance muscle growth, red blood cell production, and oxygen delivery to muscles.
Side Effects of Anabolic Steroids:
Effects in Females:
- Masculinization: Development of male characteristics, such as facial hair growth, deepening of voice, and enlargement of the clitoris.
- Increased aggressiveness: Heightened aggression and irritability.
- Mood swings and depression: Emotional instability and depressive symptoms.
- Abnormal menstrual cycles: Disruption of the menstrual cycle, including irregular periods or cessation of menstruation.
- Excessive hair growth: Increased hair growth on the face and body.
- Enlargement of clitoris: Growth of the clitoris, leading to discomfort and changes in sexual function.
Effects in Males:
- Acne: Skin condition characterized by pimples and inflammation.
- Increased aggressiveness: Heightened aggression and irritability.
- Mood swings and depression: Emotional instability and depressive symptoms.
- Reduction of testicle size: Shrinking of the testicles due to decreased natural testosterone production.
- Decreased sperm production: Impaired fertility and reduced sperm count.
- Kidney and liver dysfunction: Damage to the kidneys and liver due to prolonged steroid use.
- Breast enlargement: Growth of breast tissue in males (gynecomastia).
- Premature baldness: Early onset of male pattern baldness.
- Enlargement of the prostate gland: Increased risk of prostate enlargement and related complications.
Prevention and Control:
- Avoidance: Refrain from using drugs, including tobacco, alcohol, and illicit substances, from a young age.
- Identify risk factors: Recognize situations and environments that may contribute to the development of addiction or substance abuse.
- Seek support: Reach out to parents, teachers, and other trusted individuals for guidance and assistance in addressing substance abuse issues.




0 Comments